Quality and Saftey
Severity of illness measures: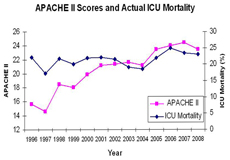
The Intensive Care Department is committed to provide high-level care up to the international standards. In doing so, the department’s performance is monitored by an internally maintained database containing information about patients´ demographics, admission diagnoses and procedures. The database also contains data about severity of illness measured by Internationally validated scoring systems. These systems are: Acute Physiology and Chronic Health Evaluation II (APACHE II); Simplified Acute Physiology Score (SAPS); Mortality Prediction Model II-0 (MPM0); Mortality Prediction Model II-24 (MPM24); and Injury Severity Score (ISS). These systems are used to predict mortality in the unit. The performance of the unit is evaluated by comparing the predicted mortality to actual mortality.
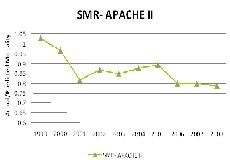
Acutal Predicted Hospital Mortality (APACHE II):
Data on actual/predicted mortality is available now for last nine years. It shows that KFNGH ICU is up to the international standards. Furthermore, the performance improved further with actual hospital mortality being less than the predicted mortality.
Quality Indicators:
The department follows 3 quality indicators: 
Ventilator Associated Pneumonia (VAP) Rate:
The department monitor the VAP rate on continuous basis as per as the NHSN criteria and in collaboration with the Infection Control Department. The rate of VAP has reduced in 2008 compared to 2007 due to multiple interventions.
ICU re-admission rate / 1000 discharges:
 ICU readmission rate is monitored as part of the ICU quality management. The overall rate has dropped from 3.1/100 discharges in 2007 to 2.2/100 discharges in 2008.
ICU readmission rate is monitored as part of the ICU quality management. The overall rate has dropped from 3.1/100 discharges in 2007 to 2.2/100 discharges in 2008.
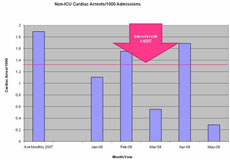
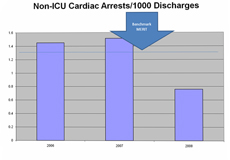
Cardiac Arrests on Medical/Surgical/OB Wards :
After implementation of the CCRT, the number of cardiac arrests of the medical and surgical / OB Wards dropped by almost 50%.
VAP Bundle Compliance (July to September 2008):
Computerized Physician Order Entry (CPOE):
CPOE is the computer system that allows direct entry of medical orders by the physician. This system reduces errors by minimizing the ambiguity of hand-written orders and by integration with patient information, including laboratory and prescription data. The order is then automatically checked for potential errors or problems. The system has been implemented in the KAMC ICU since Dec 4/2006.
High Fidelity Critical Care Simulation:

The Intensive Care Department launched the first Critical Care Simulation Center in the Region. Simulation has become the focus for improvement of patient safety and enhancing training. Crisis management training improves technical skills of individuals and crisis management behaviors and teamwork. Compared to traditional training simulation improves safety, efficacy (exposure to diverse patient conditions) and integration of multiple skills. Additionally, it provides the tool for objective & immediate feedback and is useful as assessment tool.
Our simulation lab opened in April 2008. The lab consists of one high fidelity patient Simulator which is a high tech patient simulator (SimMan) and six partial task trainers for airway management and central venous catheterization.
The simulator can simulate with high fidelity a critically ill patient in the ICU. The simulator can breath, talk, and is fully monitored. Procedures like orotracheal intubation, defibrillation, needle decompression, chest tube placement and surgical cricothyrodotomy can be performed on the simulator.
The lab is a place where health-care teams practice hands-on emergency and intensive care interventions and techniques. The goal of simulation education is to strengthen health care performance in order to enhance patient care. The simulated environment provides the experience needed without putting patients at risk and help health care professionals perfect their skills.
Simulation center activities:
 The center features a variety of simulation exercises, so residents can actively practice their skills and apply their knowledge in realistic scenarios.
The center features a variety of simulation exercises, so residents can actively practice their skills and apply their knowledge in realistic scenarios.
Residents rotating in the ICU will practice airway management and central venous catheterization on mannequins before performing the procedure on real patients.
Also residents have to run medical scenarios on the patient simulator. Following the simulation, the team reviews the exercise with a mentor. They discuss what happened, what went well and what could have gone better. They watch a video of the exercise to see themselves in action, and they discuss with their mentor what they learned individually and as a team. In addition to improving their medical knowledge in critical care medicine, they learn crisis resource management and the dynamics of team leadership and teamwork.